New Approaches to Combatting Antibiotic Resistance
In recent years, the issue of antibiotic resistance has escalated into a significant public health crisis, threatening our ability to treat common infections effectively. As bacteria evolve and adapt, the medications designed to combat them become less effective, leading to longer hospital stays, higher medical costs, and increased mortality. But fear not! Innovative strategies are emerging to combat this growing problem, and they are as exciting as they are essential. From novel antibiotic development to alternative treatment strategies, the landscape of infection control is evolving rapidly.
Imagine a world where infections that once seemed minor can be treated with ease and where the fear of resistant bacteria becomes a relic of the past. This vision is not merely a dream; it's becoming a reality as researchers and healthcare professionals join forces to tackle this global challenge. By exploring new methodologies and fostering international collaboration, we can develop effective solutions and safeguard our health.
One of the most promising avenues being explored is the development of novel antibiotics. Traditional antibiotics have served us well for decades, but their effectiveness is waning. Researchers are now focusing on discovering new compounds that can outsmart resistant bacteria. This journey is fraught with challenges, including the lengthy and expensive process of bringing new drugs to market. However, the potential rewards are enormous, as these new antibiotics could save lives and restore our faith in modern medicine.
Moreover, as we delve deeper into the intricacies of bacterial behavior, we uncover alternative treatment strategies that can augment or even replace traditional antibiotics. For instance, phage therapy is gaining traction as a viable option for targeting resistant bacteria. This method utilizes bacteriophages—viruses that specifically infect bacteria—to eliminate infections. The science behind phage therapy is fascinating; these tiny agents are like guided missiles, homing in on their bacterial targets while leaving human cells unharmed.
In addition to phage therapy, probiotics and immunotherapies are emerging as powerful allies in the fight against infections. Probiotics, often referred to as "good bacteria," can help restore the natural balance of gut flora, which is crucial for a robust immune response. By enhancing our body's natural defenses, probiotics can play a significant role in preventing infections and supporting recovery from antibiotic treatments.
On the other hand, immunotherapy represents a cutting-edge approach that seeks to boost the body’s own immune system to fight infections more effectively. This innovative strategy holds great promise, particularly for patients facing antibiotic-resistant infections. By harnessing the power of our immune system, we can potentially turn the tide against even the most stubborn bacterial foes.
As we look ahead, the importance of global collaboration cannot be overstated. Tackling antibiotic resistance is a collective effort that requires input from researchers, healthcare professionals, policymakers, and the public. By sharing knowledge and resources, we can accelerate the development of new treatments and implement effective strategies for antibiotic stewardship. This collaborative spirit is essential for building a healthier future and ensuring that antibiotics remain effective for generations to come.
- What is antibiotic resistance? Antibiotic resistance occurs when bacteria evolve to resist the effects of antibiotics, making infections harder to treat.
- How can we combat antibiotic resistance? Strategies include developing new antibiotics, implementing antibiotic stewardship programs, and exploring alternative treatments like phage therapy and probiotics.
- What is phage therapy? Phage therapy uses bacteriophages to target and kill specific bacteria, offering a potential alternative to traditional antibiotics.
- Are probiotics effective in preventing infections? Yes, probiotics can help restore gut flora balance and enhance the immune response, potentially preventing infections.
- Why is global collaboration important? Global collaboration allows for the sharing of knowledge and resources, which is crucial for developing effective solutions to tackle antibiotic resistance.

Understanding Antibiotic Resistance
Antibiotic resistance is a growing concern in the field of medicine, and it occurs when bacteria evolve to resist the effects of medications that once effectively killed them. This phenomenon is not just a scientific curiosity; it's a pressing public health crisis that can lead to longer hospital stays, higher medical costs, and increased mortality. Imagine a world where common infections become untreatable, where minor surgeries carry significant risks, and where the very medications that have saved countless lives are rendered ineffective. It's a chilling thought, isn't it?
At its core, antibiotic resistance is driven by a variety of factors, including the overuse and misuse of antibiotics in both humans and animals. When antibiotics are prescribed unnecessarily or not taken as directed, bacteria can adapt and develop resistance. This is akin to a game of survival, where only the strongest bacteria survive the onslaught of antibiotics, leading to a population of superbugs that are harder to eliminate.
To better understand how this resistance develops, it’s essential to grasp the mechanisms behind it. Bacteria can acquire resistance through several pathways:
- Mutation: Random changes in bacterial DNA can lead to resistance.
- Horizontal Gene Transfer: Bacteria can share resistance genes with one another, spreading resistance rapidly.
- Selective Pressure: The use of antibiotics creates a selective environment where only resistant bacteria thrive.
This combination of factors creates a perfect storm for the emergence and spread of antibiotic-resistant bacteria. The implications for public health are staggering. According to the World Health Organization (WHO), antibiotic resistance could lead to 10 million deaths annually by 2050 if no action is taken. This statistic should serve as a wake-up call, urging us to rethink our approach to antibiotic use and explore innovative solutions.
Moreover, the impact of antibiotic resistance extends beyond individual health. It threatens the effectiveness of modern medicine, including surgeries, chemotherapy, and organ transplants, all of which rely on effective antibiotics to prevent and treat infections. In a sense, antibiotic resistance is not just a medical issue; it’s a societal challenge that requires a collective response.
In summary, understanding antibiotic resistance is crucial for anyone who wants to grasp the complexities of modern healthcare. As we delve deeper into this topic, we will explore various strategies and innovative treatments aimed at combatting this critical challenge. By raising awareness and fostering collaboration among healthcare professionals, researchers, and the public, we can work together to turn the tide against antibiotic resistance.

Novel Antibiotic Development
As the battle against antibiotic resistance intensifies, researchers are stepping up their game to develop novel antibiotics that can outsmart the evolving bacteria. The urgency of this endeavor cannot be overstated; with each passing day, more infections are becoming resistant to existing treatments, leaving healthcare professionals scrambling for solutions. So, what’s the latest in the world of antibiotic development? Let’s dive into some groundbreaking advancements and the hurdles that researchers face along the way.
One of the most exciting avenues being explored is the use of natural compounds. Scientists are scouring the globe, from the depths of the ocean to the canopies of rainforests, searching for microorganisms that produce unique substances capable of killing bacteria. For instance, researchers have identified a rare bacterium in a remote cave that produces a potent antibiotic, which could potentially serve as a template for new drug development. This approach not only taps into the vast biodiversity of our planet but also emphasizes the importance of preserving these ecosystems for future medical discoveries.
However, the path to bringing new antibiotics to market is fraught with challenges. The regulatory landscape is complex, and the process can take over a decade. The lengthy timeline is often a deterrent for pharmaceutical companies, especially when the financial return on investment is uncertain. To illustrate this point, consider the following table that outlines the typical stages of antibiotic development:
| Stage | Description | Average Duration (Years) |
|---|---|---|
| Discovery | Identifying potential compounds through screening and testing. | 3-6 |
| Preclinical Testing | Laboratory testing on animals to assess safety and efficacy. | 1-3 |
| Clinical Trials | Human testing in three phases to evaluate safety, dosage, and effectiveness. | 3-7 |
| Regulatory Review | Submission of data to regulatory bodies for approval. | 1-2 |
| Market Launch | Introduction of the antibiotic to the market. | Varies |
Despite these challenges, innovative strategies are emerging to expedite the antibiotic development process. For example, researchers are increasingly utilizing artificial intelligence (AI) to sift through vast databases of chemical compounds and predict which ones might be effective against resistant bacteria. This technology not only speeds up the discovery phase but also enhances the accuracy of predictions, potentially leading to faster development timelines.
Moreover, collaborations between academic institutions, biotechnology firms, and pharmaceutical companies are becoming more common. By pooling resources and expertise, these partnerships can tackle the multifaceted challenges of antibiotic development more effectively. For instance, a recent collaboration between a university and a biotech company led to the rapid development of a new antibiotic that targets a particularly stubborn strain of bacteria, showcasing the power of teamwork in this critical field.
In conclusion, while the journey of developing novel antibiotics is fraught with obstacles, the passion and innovation of researchers worldwide are shining a light on potential solutions. The quest for new antibiotics is not just about creating drugs; it’s about safeguarding public health for future generations. As we continue to explore these novel approaches, it’s essential to remain optimistic and supportive of the scientific community’s efforts to combat antibiotic resistance.
- What are novel antibiotics? Novel antibiotics are new drugs developed to combat bacterial infections, especially those resistant to existing treatments.
- Why is antibiotic resistance a problem? Antibiotic resistance makes infections harder to treat, leading to longer hospital stays, higher medical costs, and increased mortality.
- How can we support antibiotic development? Supporting research initiatives, advocating for policy changes, and practicing responsible antibiotic use can all help in the fight against antibiotic resistance.
Phage Therapy
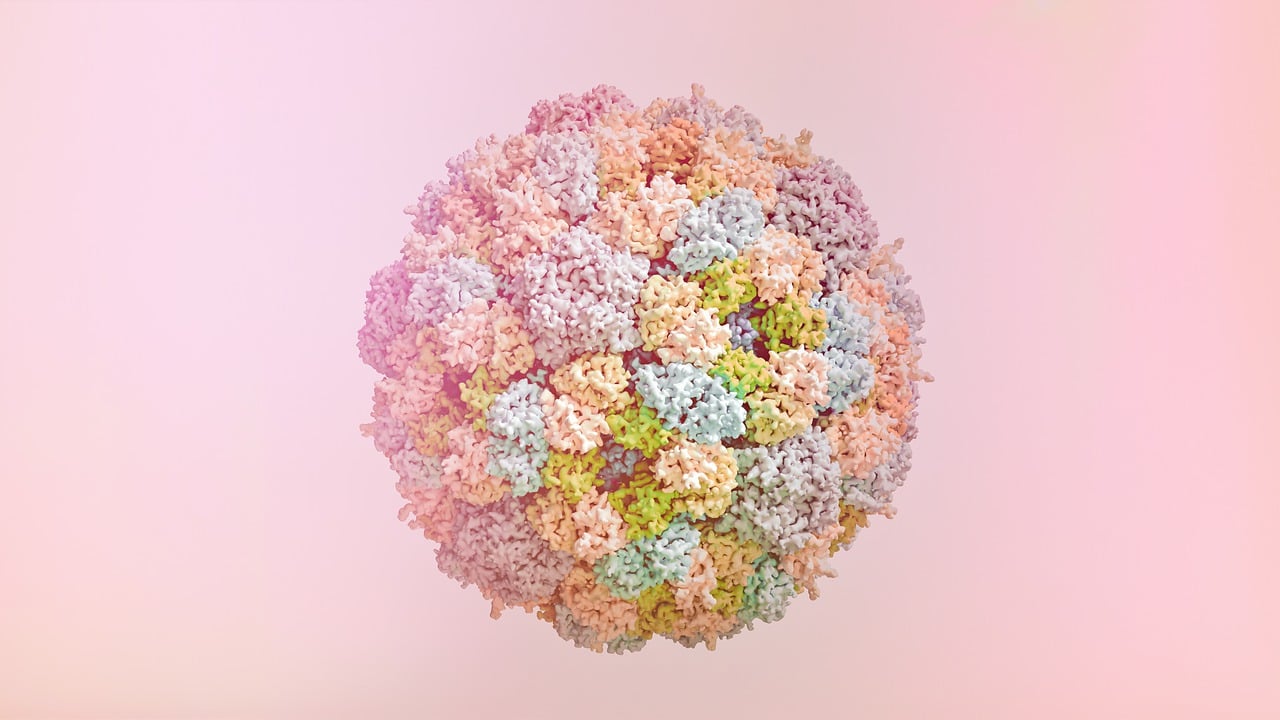
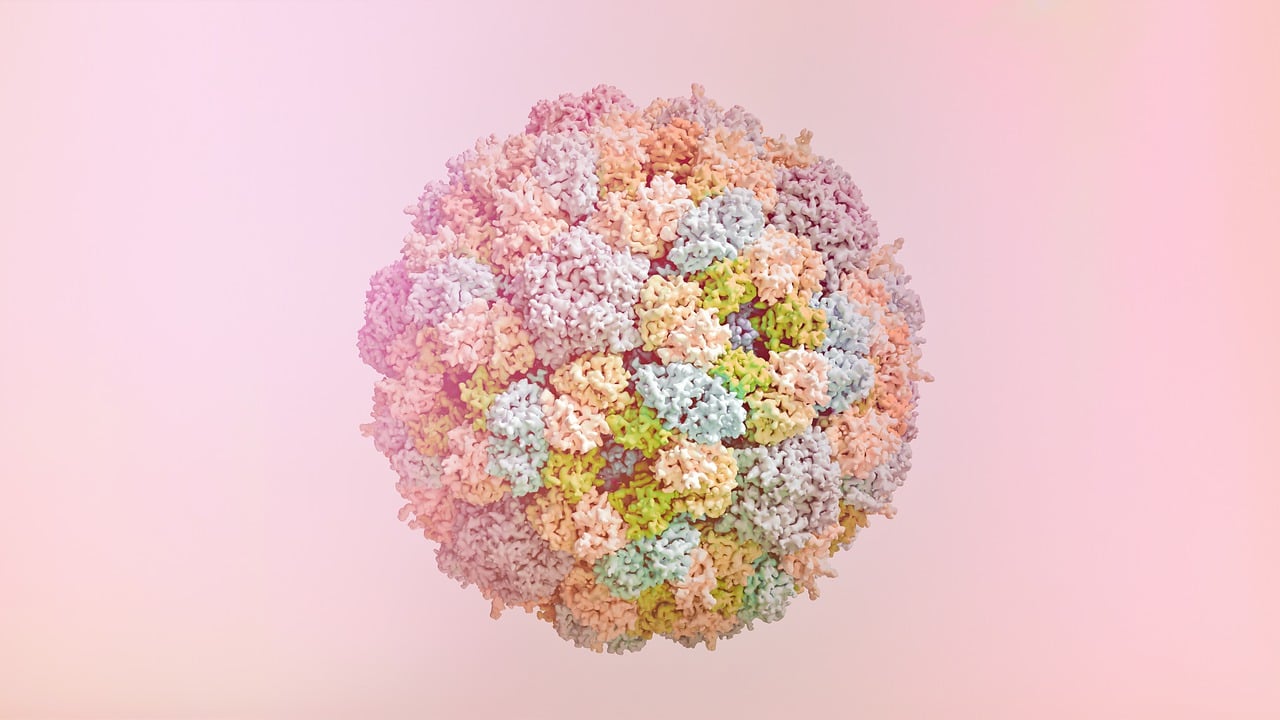
Phage therapy is a groundbreaking approach that harnesses the power of bacteriophages—viruses that specifically infect bacteria—to combat antibiotic-resistant infections. Imagine these phages as tiny, precision-guided missiles, designed to seek out and destroy their bacterial targets without harming human cells or beneficial microbes. This innovative treatment has gained traction in recent years, especially as traditional antibiotics become less effective against evolving bacterial strains. The beauty of phage therapy lies in its specificity; unlike broad-spectrum antibiotics that can disrupt the entire microbiome, phages can be tailored to target only the harmful bacteria causing an infection.
The potential of phage therapy is enormous, particularly as we face a public health crisis marked by rising antibiotic resistance. Current research is exploring various applications of phages in clinical settings, with a focus on their practical use against infections that resist conventional treatments. For instance, studies have shown that phage therapy can be effective in treating chronic wounds, respiratory infections, and even certain gastrointestinal infections. As we delve deeper into this fascinating field, it becomes clear that phage therapy could be a game changer in the fight against resistant bacteria.
However, the journey to widespread acceptance and implementation of phage therapy is not without challenges. Regulatory hurdles, production scalability, and the need for rigorous clinical trials to ensure safety and efficacy are just a few of the obstacles researchers face. Moreover, the variability of phage preparations—since phages can differ in their effectiveness against the same bacterial strain—adds another layer of complexity to their use. Despite these challenges, the excitement surrounding phage therapy is palpable, and researchers are working tirelessly to overcome these barriers.
As we explore the mechanisms of phage action, it's essential to understand how these viruses can effectively disrupt bacterial cell functions. Phages can employ various strategies, including:
- Adsorption: Phages attach to specific receptors on the bacterial surface.
- Pentration: Once attached, they inject their genetic material into the host bacterium.
- Replication: The phage's genetic material hijacks the bacterial machinery to produce new phage particles.
- Lysis: Finally, the newly formed phages cause the bacterium to burst, releasing the phages to infect other bacteria.
This multi-step process not only highlights the efficiency of phage therapy but also underscores its potential as a targeted treatment option. As ongoing research continues to unveil the intricacies of phage therapy, we can anticipate a future where this method could become a cornerstone in our arsenal against antibiotic-resistant infections. In the following sections, we will explore successful case studies and ongoing clinical trials that further demonstrate the effectiveness of phage therapy in real-world settings.
- What is phage therapy? Phage therapy is the use of bacteriophages to treat bacterial infections, particularly those resistant to antibiotics.
- How does phage therapy work? Phages attach to bacteria, inject their genetic material, replicate inside the bacteria, and ultimately cause the bacteria to burst, releasing new phages.
- Is phage therapy safe? While phage therapy has shown promise in clinical trials, more research is needed to fully understand its safety and efficacy.
- Where is phage therapy currently being used? Phage therapy is not yet widely available but is being explored in various clinical trials and has been used in some compassionate use cases.
Mechanisms of Phage Action
Understanding the is crucial in the quest to harness bacteriophages as a viable alternative to traditional antibiotics. Bacteriophages, or phages for short, are viruses that specifically infect and kill bacteria. Unlike antibiotics that can affect a wide range of bacteria, phages are highly selective. This specificity can be a double-edged sword; while it allows for targeted treatment, it also necessitates a deep understanding of how these phages operate to ensure their effectiveness.
Phages employ several mechanisms to destroy bacteria, and these can be categorized into a few key processes:
- Adsorption: The first step in the phage lifecycle is the attachment to a bacterial cell. Phages recognize specific receptors on the surface of bacteria. This interaction is akin to a key fitting into a lock, where only the right phage can attach to its corresponding bacterial host.
- Pentration: Once attached, the phage injects its genetic material into the bacterial cell. This process is similar to a syringe injecting medicine into a patient, where the phage's DNA takes control of the bacterial machinery.
- Replication: Inside the bacterial cell, the phage's genetic material hijacks the bacteria's cellular processes to replicate itself. The bacteria effectively become a factory, producing new phage particles instead of its own components.
- Lysis: Finally, the newly formed phages cause the bacterium to burst open, or lyse, releasing new phages into the environment to infect other bacterial cells. This dramatic explosion can be visualized as a balloon popping, scattering its contents everywhere.
This cycle not only leads to the death of the targeted bacteria but also reduces the population of harmful pathogens in the body. However, it's important to note that phage therapy is not without its challenges. The evolution of bacteria can lead to the emergence of phage-resistant strains, which is why ongoing research is essential to stay one step ahead in this battle against antibiotic resistance.
In addition to these mechanisms, researchers are investigating how phages can be combined with other treatments to enhance their effectiveness. For example, using phages alongside antibiotics may help to overcome resistance by targeting bacteria that are less susceptible to conventional treatments. This synergistic approach could revolutionize the way we manage bacterial infections.
As we delve deeper into the world of phage therapy, understanding these mechanisms will be key to developing effective treatments against antibiotic-resistant infections. The future of infection management may very well depend on our ability to leverage these tiny viral warriors in the fight against one of the most pressing public health challenges of our time.
- What are bacteriophages? Bacteriophages, or phages, are viruses that specifically infect and kill bacteria.
- How do phages work? Phages attach to bacterial cells, inject their genetic material, replicate inside the bacteria, and eventually cause the bacteria to burst open, releasing new phages.
- Are phages safe for humans? Phage therapy has shown promise in clinical trials, but more research is needed to fully understand its safety and efficacy in humans.
- Can phages be used alongside antibiotics? Yes, combining phages with antibiotics may help enhance treatment effectiveness and overcome bacterial resistance.

Clinical Applications of Phage Therapy
Phage therapy is rapidly gaining traction as a viable alternative to traditional antibiotics, particularly in the face of rising antibiotic resistance. This innovative approach leverages the natural ability of bacteriophages—viruses that specifically infect bacteria—to target and destroy harmful bacterial pathogens. The clinical applications of phage therapy are both promising and diverse, with numerous case studies and ongoing trials demonstrating its effectiveness in treating various infections.
One of the most compelling aspects of phage therapy is its specificity. Unlike broad-spectrum antibiotics that can indiscriminately kill both harmful and beneficial bacteria, phages are selective, targeting only the bacteria responsible for the infection. This specificity not only minimizes collateral damage to the microbiome but also reduces the likelihood of developing further resistance. For instance, a recent clinical trial involving a patient with a severe multi-drug resistant (MDR) infection showcased the power of phage therapy. After exhausting all conventional treatment options, the patient was administered a tailored phage preparation, resulting in a significant reduction of the infection and an overall improvement in health.
Moreover, phage therapy has shown remarkable success in treating chronic infections, particularly those associated with biofilms—clusters of bacteria that adhere to surfaces and are notoriously difficult to eradicate. A notable example is the treatment of chronic osteomyelitis, a persistent bone infection where biofilms are often present. In cases where antibiotics failed, phage therapy has not only cleared the infection but also facilitated healing, showcasing its potential as a game-changer in managing chronic conditions.
As we delve deeper into the clinical applications of phage therapy, it’s essential to highlight the importance of personalized treatment. Phages can be isolated and characterized from the patient's own microbiome or from environmental sources, allowing for a customized approach that targets the specific bacterial strain causing the infection. This personalized medicine aspect is crucial, as it addresses the unique characteristics of each patient's infection, leading to more effective treatment outcomes.
In addition to individual cases, there are broader implications for public health. Phage therapy not only provides an alternative for patients suffering from antibiotic-resistant infections but also contributes to the global fight against antibiotic resistance. By reducing reliance on traditional antibiotics, phage therapy can help preserve the efficacy of existing antibiotics, ensuring they remain effective for future generations.
However, while the clinical applications of phage therapy are promising, it is essential to approach this treatment modality with careful consideration. Regulatory challenges, standardization of phage preparations, and the need for rigorous clinical trials remain obstacles that must be addressed to fully integrate phage therapy into mainstream medical practice. As researchers continue to explore and refine phage therapy, the hope is that it will complement existing treatment options and provide a robust arsenal against the ever-evolving threat of antibiotic resistance.
In conclusion, the clinical applications of phage therapy represent a beacon of hope in the battle against antibiotic-resistant infections. With ongoing research and successful case studies paving the way, this innovative treatment could soon become a cornerstone of infection management, reshaping the future of healthcare.
- What is phage therapy? Phage therapy is a treatment that uses bacteriophages—viruses that infect bacteria—to target and kill specific bacterial pathogens, especially those resistant to antibiotics.
- How does phage therapy differ from antibiotics? Unlike antibiotics that can affect a wide range of bacteria, phage therapy is highly specific, targeting only the bacteria causing the infection, which helps preserve beneficial bacteria in the microbiome.
- Is phage therapy safe? Current research indicates that phage therapy is generally safe, but like any medical treatment, it must be administered under professional supervision, especially since it is still being studied and developed.
- Where is phage therapy currently being used? Phage therapy is being explored in various clinical settings worldwide, particularly for patients with multi-drug resistant infections and chronic conditions where conventional treatments have failed.

Antibiotic Stewardship Programs
Antibiotic stewardship programs (ASPs) are essential initiatives designed to optimize the use of antibiotics in healthcare settings. The primary goal of these programs is to ensure that patients receive the most appropriate antibiotic treatment, reducing the risk of developing antibiotic resistance. Imagine a world where antibiotics still work effectively; that’s the vision ASPs strive to achieve. By promoting the judicious use of these powerful drugs, we can help preserve their efficacy for future generations.
ASPs operate on several key principles. First, they emphasize the importance of accurate diagnosis. When healthcare providers can pinpoint the exact cause of an infection, they can prescribe the right antibiotic, if needed, rather than resorting to broad-spectrum options that can contribute to resistance. Additionally, ASPs encourage the use of the narrowest spectrum of antibiotics possible, targeting specific pathogens while sparing beneficial bacteria.
Implementing an effective antibiotic stewardship program involves various strategies, including:
- Education and Training: Healthcare professionals need ongoing education about the importance of antibiotic stewardship, including the latest guidelines and resistance patterns.
- Monitoring and Feedback: Regularly reviewing antibiotic prescribing patterns and providing feedback to prescribers helps identify areas for improvement.
- Guideline Development: Establishing evidence-based guidelines for antibiotic use can standardize practices and ensure that all patients receive optimal care.
Moreover, the impact of these programs extends beyond individual patient care. By reducing unnecessary antibiotic prescriptions, ASPs contribute to a broader public health strategy aimed at combating antibiotic resistance. Studies have shown that hospitals with robust stewardship programs see a significant decrease in antibiotic use, which in turn correlates with lower rates of resistant infections.
However, implementing ASPs is not without challenges. One major hurdle is the need for institutional support and resources. Hospitals must invest in training, monitoring systems, and dedicated personnel to oversee the program's success. Additionally, there can be resistance from healthcare providers who may feel that their prescribing autonomy is being challenged. Overcoming these obstacles requires strong leadership and a culture of collaboration among healthcare teams.
In conclusion, antibiotic stewardship programs are a crucial component in the fight against antibiotic resistance. By promoting responsible antibiotic use and fostering a culture of awareness, we can protect the effectiveness of these vital medications. The journey towards effective stewardship is ongoing, but with collective effort, we can pave the way for a healthier future.
Q: What are the main goals of antibiotic stewardship programs?
A: The main goals are to optimize antibiotic use, reduce the incidence of antibiotic resistance, and improve patient outcomes by ensuring appropriate treatment.
Q: How can healthcare providers contribute to antibiotic stewardship?
A: Providers can contribute by adhering to guidelines, participating in training sessions, and actively engaging in monitoring and feedback processes.
Q: What impact do antibiotic stewardship programs have on public health?
A: ASPs help reduce the overall use of antibiotics, which decreases the prevalence of antibiotic-resistant infections, ultimately benefiting public health.

Alternative Treatment Strategies
As the battle against antibiotic resistance escalates, researchers and healthcare professionals are turning their attention to that go beyond traditional antibiotics. These innovative approaches not only aim to combat resistant infections but also work towards enhancing overall patient health. With the increasing recognition that antibiotics are not the only solution, a diverse range of methods is emerging, each with its unique benefits and mechanisms of action.
One of the most promising areas in alternative treatment is the use of probiotics. These live microorganisms, often referred to as "good bacteria," play a crucial role in maintaining gut health. By restoring the natural balance of flora in our intestines, probiotics can enhance the immune response, potentially preventing infections from taking hold. Imagine your gut as a bustling city; when good bacteria are thriving, it keeps the bad ones at bay, much like a well-functioning police force. Recent studies suggest that probiotics can not only help in the recovery from antibiotic treatments but may also reduce the incidence of infections in the first place.
On the other hand, immunotherapy is gaining traction as a game-changer in infection control. This treatment strategy focuses on boosting the body's natural defenses, enabling it to fight off infections more effectively. Rather than relying solely on external medications, immunotherapy empowers the immune system to recognize and eliminate pathogens. Think of it as training a team of elite soldiers (your immune cells) to recognize and tackle the enemy (bacteria) more efficiently. Recent advancements in this field have shown promise, with therapies being developed that target specific bacteria and enhance the immune response against them.
Moreover, the integration of these alternative strategies into existing treatment protocols has the potential to revolutionize how we approach infections. For instance, combining probiotics with conventional antibiotic treatments could mitigate some of the adverse effects associated with antibiotics, such as gut dysbiosis. This synergy not only enhances treatment outcomes but also contributes to a more holistic approach to patient care.
However, while the potential of these alternative treatments is significant, ongoing research is crucial. Understanding the precise mechanisms through which probiotics and immunotherapies work will help refine these strategies and ensure their effectiveness. As we continue to explore these avenues, the importance of clinical trials cannot be overstated. They provide the necessary data to validate these methods and pave the way for their acceptance in mainstream medicine.
In summary, the landscape of infection treatment is evolving rapidly. With the rise of antibiotic resistance, embracing alternative treatment strategies like probiotics and immunotherapy is not just a possibility; it’s becoming a necessity. By diversifying our approach, we can enhance patient outcomes and build a more resilient healthcare system capable of tackling the challenges posed by resistant infections.
- What are probiotics, and how do they work? Probiotics are beneficial bacteria that help maintain a healthy balance in the gut, enhancing the immune system and potentially preventing infections.
- How does immunotherapy differ from traditional antibiotics? Immunotherapy boosts the body's own immune response to fight infections, while antibiotics directly kill or inhibit the growth of bacteria.
- Can probiotics be used alongside antibiotics? Yes, probiotics can be taken during or after antibiotic treatment to help restore gut flora and reduce side effects.
- Are there any risks associated with alternative treatments? Like any treatment, alternative therapies can have side effects or interactions, so it's essential to consult healthcare providers before starting any new regimen.

Probiotics and Gut Health
When we talk about probiotics, we're diving into a fascinating world of tiny heroes that play a monumental role in our gut health. These live microorganisms, often referred to as "good bacteria," can be found in various foods and supplements. But why should we care about them? Well, imagine your gut as a bustling city, filled with both friendly and unfriendly inhabitants. Probiotics are like the peacekeepers that help maintain harmony in this city, ensuring that the good bacteria thrive while keeping the bad ones at bay.
Research has shown that a well-balanced gut microbiome is crucial for overall health. Probiotics contribute to this balance by enhancing the body’s natural defenses against infections. They do this by competing with harmful bacteria for resources and producing substances that inhibit their growth. So, when you consume probiotics, you're essentially sending in reinforcements to your gut army, ready to combat any invading pathogens. Some studies even suggest that probiotics can reduce the duration and severity of gastrointestinal infections, making them a valuable ally in our quest for health.
But the benefits of probiotics extend beyond just fighting off infections. They also play a significant role in digestive health. By helping to break down food and absorb nutrients, probiotics ensure that our bodies get the most out of what we eat. This is particularly important when we're on antibiotics, which can disrupt the natural balance of our gut flora. During such times, incorporating probiotics can help restore that balance and prevent issues like diarrhea, which is a common side effect of antibiotic treatment.
So, what are some of the best sources of probiotics? You might be surprised to learn that they can be found in a variety of delicious foods. Here’s a quick list of probiotic-rich foods that you might want to include in your diet:
- Yogurt: A popular source, especially if it contains live and active cultures.
- Kefir: A fermented dairy product that's even richer in probiotics than yogurt.
- Sauerkraut: Fermented cabbage that not only adds flavor but also boosts gut health.
- Kombucha: A fizzy drink made from fermented tea, packed with probiotics.
- Miso: A fermented soybean paste used in soups and sauces, full of beneficial bacteria.
Incorporating these foods into your diet can be a simple yet effective way to enhance your gut health. However, it’s essential to remember that not all probiotics are created equal. Different strains of probiotics have different effects, and what works for one person may not work for another. Therefore, it’s a good idea to consult with a healthcare professional before starting any new supplement regimen.
In conclusion, probiotics serve as crucial allies in maintaining gut health, particularly in the face of antibiotic use and infections. By understanding their role and incorporating them into our diets, we can harness their power to promote a balanced gut microbiome and enhance our overall well-being. So, the next time you enjoy a bowl of yogurt or sip on some kombucha, remember that you’re not just indulging in a tasty treat; you’re also fortifying your gut defenses!
1. What are probiotics?
Probiotics are live microorganisms, often referred to as "good bacteria," that provide health benefits when consumed in adequate amounts.
2. How do probiotics help with gut health?
Probiotics help maintain a balanced gut microbiome, enhance digestion, and support the body’s natural defenses against harmful bacteria.
3. Can probiotics prevent side effects of antibiotics?
Yes, probiotics can help restore gut flora balance and may prevent diarrhea and other gastrointestinal issues that can arise from antibiotic use.
4. Are all probiotic foods equally effective?
No, different strains of probiotics have different effects, and their efficacy can vary from person to person. It's essential to find the right strains that work for you.

Immunotherapy in Infection Control
Immunotherapy is rapidly emerging as a groundbreaking approach in the battle against antibiotic-resistant infections. Unlike traditional antibiotics that directly target bacteria, immunotherapy aims to enhance the body’s own immune response to effectively combat infections. This innovative strategy is akin to training an army to fight more efficiently rather than sending in more troops. By empowering the immune system, we can potentially turn the tide against stubborn pathogens that have developed resistance to conventional treatments.
One of the most exciting aspects of immunotherapy is its versatility. Various techniques are being explored, including monoclonal antibodies, vaccines, and immune checkpoint inhibitors. For instance, monoclonal antibodies can be designed to specifically target and neutralize harmful bacteria or their toxins. This method not only helps in clearing the infection but also minimizes collateral damage to beneficial bacteria, which is often a downside of traditional antibiotics.
Additionally, vaccines play a crucial role in preventing infections before they occur. By training the immune system to recognize and respond to specific pathogens, vaccines can significantly reduce the incidence of infections. This preventative approach is particularly important in the context of antibiotic resistance, as it decreases the need for antibiotic use in the first place. Imagine a world where vaccines can prevent infections that currently require aggressive antibiotic treatments—this could dramatically lessen the burden of resistance.
Moreover, researchers are investigating the use of immune checkpoint inhibitors, which are already making waves in cancer treatment. These inhibitors work by blocking proteins that prevent the immune system from attacking the bacteria effectively. By unleashing the immune system's full potential, we could see a new era of treatment options for infections that have become nearly untreatable.
However, the journey toward integrating immunotherapy into standard infection control practices is not without its challenges. Clinical trials are essential for determining the efficacy and safety of these therapies. The complexity of the immune system means that responses can vary significantly from person to person, and finding the right balance in treatment is crucial. As researchers continue to explore these avenues, the hope is to establish protocols that can be widely adopted in clinical settings.
In conclusion, immunotherapy represents a promising frontier in the fight against antibiotic-resistant infections. By harnessing the power of the immune system, we can potentially offer new hope to patients suffering from infections that have long resisted treatment. As we continue to invest in research and development in this field, the dream of a more effective and sustainable approach to infection control may soon become a reality.
- What is immunotherapy? Immunotherapy is a treatment that uses the body's own immune system to fight infections and diseases, including antibiotic-resistant infections.
- How does immunotherapy differ from traditional antibiotics? Unlike antibiotics that kill bacteria directly, immunotherapy enhances the immune response to help the body fight off infections more effectively.
- Are there any risks associated with immunotherapy? As with any medical treatment, there are potential risks and side effects. It's important to discuss these with a healthcare provider.
- What types of immunotherapy are currently being researched for infection control? Research is ongoing into monoclonal antibodies, vaccines, and immune checkpoint inhibitors as potential treatments for antibiotic-resistant infections.
Frequently Asked Questions
- What is antibiotic resistance?
Antibiotic resistance occurs when bacteria evolve to resist the effects of medications designed to kill them. This evolution makes infections harder to treat, leading to prolonged illness, increased healthcare costs, and a greater risk of death.
- How do bacteria become resistant to antibiotics?
Bacteria can become resistant through various mechanisms, such as genetic mutations or acquiring resistance genes from other bacteria. Overuse and misuse of antibiotics in humans and agriculture accelerate this process, allowing resistant strains to thrive.
- What are the new approaches to combat antibiotic resistance?
Innovative strategies include developing novel antibiotics, utilizing phage therapy, and implementing antibiotic stewardship programs. These approaches aim to optimize antibiotic use and explore alternative treatments to tackle resistant infections.
- What is phage therapy?
Phage therapy is the use of bacteriophages, which are viruses that specifically target and kill bacteria. This method shows promise as an alternative treatment for infections caused by antibiotic-resistant bacteria.
- How effective is phage therapy?
Phage therapy has shown success in several case studies and ongoing clinical trials, demonstrating its potential to treat resistant infections effectively. However, more research is needed to fully understand its capabilities and limitations.
- What are antibiotic stewardship programs?
Antibiotic stewardship programs are initiatives designed to promote the appropriate use of antibiotics. They aim to reduce unnecessary prescriptions, improve treatment outcomes, and ultimately combat antibiotic resistance.
- Can probiotics help with antibiotic resistance?
Probiotics can help restore the balance of gut flora, potentially enhancing immune response and preventing infections. They may also support antibiotic treatment by mitigating side effects and promoting recovery.
- What role does immunotherapy play in infection control?
Immunotherapy aims to boost the body's natural defenses against infections, making it a promising approach for treating antibiotic-resistant infections. Recent developments in this field are opening new avenues for effective infection management.



















